About not using soap:
I have noticed this (an improvement) too (about 2 years ago), in a period in which I tried to use no soap on the face, and just washed the face mildly with water. I maybe only washed the face with soap after shaving, which I maybe did once every few days. But the face does become more oily and outer skin seem to stack up, making the skin less smooth and a bit flaky (but not dry flakes, more oily flakes). This could be a perfect environment for demodex: oily skin without the use of soaps. But in poor countries (and ancient times), this is probably pretty normal, and these don’t have very bad skin either. So I’m not sure whether the use of soaps is good for the skin. Soap basically reduces surface tension when combined with water, making it easier to flush off things (sebum, dirt etc) from the skin. Although sebum also keeps the skin moisturized, smooth and strong, but it also feeds demodex.
In this period, I didn’t really know about demodex. Shortly after this, I learned about demodex, and because I still had new lesions, I tried different approaches.
But I find it hard to make conclusions about this period. Why was there an improvement? Maybe it was accidentally caused by something else (for example the time of year?), maybe it was just temporary before a worsening? Some ideas/hypotheses (not sure whether these are true of false):
- By not washing and touching the face, you 1) avoid spreading bacteria from your hands (or maybe even bacteria in the soap, because soap doesn’t kill bacteria, it just flushes them away) or 2) avoid spreading bacteria or demodex on your face to other parts of the face.
- By not washing the face, your skin stays moisturized/protected and the skin doesn’t crack as easily, making it harder for bacteria such as staph to survive and penetrate the outer skin.
- By not washing the face, the skin PH stays more healthy. Skin PH is an important factor in protecting the skin against opportunistic bacteria, such as staph. PH should be below 7 (about 5) and thus should be slightly acidic, while soaps often increase skin PH (which is bad).
- By not washing the face, the environment for demodex becomes better, causing less mites to die off, which maybe improves the face temporary, but at the same time increase them in population.
The possibility of a demodex die off phase makes it extra difficult to test these hypotheses.
About tea tree oil:
Note that tea tree oil is also a skin irritant. So a worsening by using tea tree oil may be caused by demodex dying off, but also by tea tree oil irritating, or drying the skin.
In my case, I tried “tea tree oil” on the face globally with this product for just a few days: http://www.drorganic.co.uk/product-info.asp?Auto_ID=202 , which basically doesn’t contain tea tree oil, but terpinen-4-ol, the most active ingredient of tea tree oil (note that tea tree oil also contains other active ingredients, although less active). I got some irritated mouth corners from it, which I think is called angular cheilitis, something I never really had before. Strange is that people are actually using tea tree oil to combat angular cheilitis, while I got it from using it (the t4o cream). But I used it very shortly, just a few days, so I can’t really tell what it did for the yellow crusting lesions.
About my Soolantra experience:
I’m currently on day 40.
I started using Soolantra on a peak outbreak (or maybe one week after a peek) caused by the withdrawal of topical steroids. (Which I temporary used because I wanted to have a clean face on an important event, and used it for about 2 months.) This makes it difficult to compare it, because the peak outbreak by topical steroid would improve anyway back to a normal baseline (even without Soolantra). The previous time, I used it, it took about 1 month to get back to baseline, in which the first 2 weeks were the hardest. This time, the peak outbreak was about 4 days after withdrawal, with lots of bumps and itch all over the face.
I don’t know the dates exactly anymore, but roughly something like this:
- beginning of June: started with topical steroids in the face globally. (used it a bit before but more only locally on the lesions), because I wanted to be clean because of an event.
- 7 August: stopped using topical steroid
- 10-15 August: peak outbreak because of the topical steroid withdrawal (TSW). Lots of itch, bumps, followed by crusts. A lot worse than my previous withdrawal, in which I got a lot of white headed acne, but without all the bumps and crusts. Fortunately this time it was during holiday season, so I could easily stay home with some food backed up.
- about 15 August? : started using XFCream (topical 3% metronidazole)
- 18 August: start with Soolantra
- few days after 18 August: couldn’t detect demodex mites anymore by skin microscope. Reduction in itch. (Note that any improvement in this period may also be simply because of a reduction in topical steroid withdrawal symptoms.)
- about 27-31 August: skin was back to the baseline before the use of topical steroids, or maybe even better. Considering the large breakout and comparing the less severe previous TSW breakout, I recovered quicker this time than expected.
- Maybe a further improvement in the days, week after.
- But I haven’t seen any clear improvements since the last number of weeks, but I still get new lesions, although I does seem to be better than before the TSW baseline.
- Stopped using XFCream since about 2 weeks ago, but continued Soolantra. A don’t see a clear difference, with/without XFCream.
The conclusions I make about it at the moment about Soolantra:
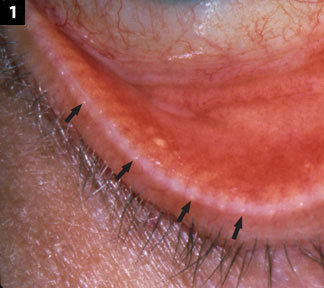
- I think Soolantra has made my eyelids healthier, even though I don’t apply it directly on the eyes. Although I didn’t had much blepharitis lately, my eyelids seems to be smoother and better colored just a few days after the start of Soolantra, and feel more moistured.
- I think Soolantra has reduced the itch on my face. I had a lot of itch during TSW, but minor itch (very localized and sporadic during the day) before TSW (baseline). But now with Soolantra, I even have less itch on the face.
- After using Soolantra, I haven’t really seen any lesions anymore at my most affected location: the right side, below the eye, horizontally at the nose level. Also, I hardly get any new lesions anymore at the area above the lip and below the nose, the mustache area.
- My skin has improved (the oozing yellow crusts improved), but because of the TSW peak, it would improve anyway. But it did improve quicker than expected. My skin seems to be better than before baseline, but it’s difficult to contribute this to Soolantra, especially because I don’t see any clear further improvements. (Or it may be going too slow to clearly notice.) If Soolantra was the cause of the quick improvement, then why doesn’t it improve further? At the moment, my skin is good (compared to baseline), but further clear improvement seems to be stuck for some weeks. Making be question whether Soolantra is really doing something to the yellow crusting problem, or whether some other factor is (also?) causing it to be below baseline. The most affected area is currently the chin, and lower left of the face. The other areas are pretty good, although I do get bumps over there without yellow crusting.
About opthomologist:
[quote]I have tracked down an opthomologist in California who actually is educated and treats for demodex. This is the place http://visionsource-advancedeye.com/1
This is the video: https://www.youtube.com/watch?v=_tm-GTTMydE2[/quote]
Not sure if in your case the problem at the eyelids it worse than the rest of the face. (In my case the face it a lot worse than problems at the eyelids, although in the beginning I did had more eyelids problems.)
But I’m not sure if opthomologists can and will easily prescribe Soolantra, compared to dermatologists, because Soolantra is used for the treatment of rosacea and because Soolantra shouldn’t be applied on the eyes (according to the manual). Although ocular rosacea also exists.
Also note that the success stories (Success stories) that used Soolantra (topical ivermectin), also used oral metronidazole. And one also used oral ivermectin.
Also note that some mites may be resistant to certain anti-parasite medication. For example, in this study:
http://www.ncbi.nlm.nih.gov/pubmed/14576651
(full text)
This patient was unresponsive to oral ivermectin and other anti mite medication, but quickly recovered on oral metronidazole. (Note that both oral ivercmectin and oral metronidazole are able to cause serious side effects.)